Intake Notes Template
Intake Notes Template - Intake questionnaires are forms that you send to clients, while treatment notes are forms you use internally to make notes on a client's timeline. Therapynotes’ intake note allows you to document a full biopsychosocial evaluation of your client, including the presenting problem, a mental status exam, and history. In this guide, we'll walk you through the steps. Templates for intake, progress notes, treatment plans and more! Collect vital client info and ensure a smooth therapy process. Optimize your practice with an intake form template for therapists. This includes creating and providing useful counseling toolkits, resources, and templates such as free counseling templates, free soap notes templates, and free counseling. Therapynotes' psychiatry intake note template allows you to capture both a robust biopsychosocial history of your patient and effectively document medical services within a. The intake assessment template simplifies the initial evaluation process, enabling quick and comprehensive capture of essential patient history and primary concerns. Unlike progress notes that track progress on ongoing treatment, intake notes are more comprehensive and capture the client's history, current situation, and treatment goals. Optimize your practice with an intake form template for therapists. The intake assessment template simplifies the initial evaluation process, enabling quick and comprehensive capture of essential patient history and primary concerns. Intake questionnaires are forms that you send to clients, while treatment notes are forms you use internally to make notes on a client's timeline. A therapy intake assessment note is a structured document used by mental health professionals to collect and organize information about a new client during the initial intake. To highlight documentation styles and content, this example contains a mix of narrative and bulleted information for each category within a template. Therapynotes' psychiatry intake note template allows you to capture both a robust biopsychosocial history of your patient and effectively document medical services within a. Each of these follow the same. Mentalyc's template builder is a powerful tool that allows therapists to create customized progress and intake note templates. Templates for intake, progress notes, treatment plans and more! In this guide, we'll walk you through the steps. Mentalyc notes cover symptoms, functioning, and include related quotes from the client, effectively conveying patient experiences as per guidewell's guidelines. Collect vital client info and ensure a smooth therapy process. In this guide, we'll walk you through the steps. Therapynotes’ intake note allows you to document a full biopsychosocial evaluation of your client, including the presenting problem, a mental status. Collect vital client info and ensure a smooth therapy process. Take advantage of our template library and focus your time where it really matters for your clients. Therapynotes' psychiatry intake note template allows you to capture both a robust biopsychosocial history of your patient and effectively document medical services within a. Mentalyc notes cover symptoms, functioning, and include related quotes. Take advantage of our template library and focus your time where it really matters for your clients. Intake questionnaires are forms that you send to clients, while treatment notes are forms you use internally to make notes on a client's timeline. Collect vital client info and ensure a smooth therapy process. Therapynotes' psychiatry intake note template allows you to capture. Templates for intake, progress notes, treatment plans and more! Unlike progress notes that track progress on ongoing treatment, intake notes are more comprehensive and capture the client's history, current situation, and treatment goals. Optimize your practice with an intake form template for therapists. Collect vital client info and ensure a smooth therapy process. Mentalyc's template builder is a powerful tool. Mentalyc notes cover symptoms, functioning, and include related quotes from the client, effectively conveying patient experiences as per guidewell's guidelines. This includes creating and providing useful counseling toolkits, resources, and templates such as free counseling templates, free soap notes templates, and free counseling. Take advantage of our template library and focus your time where it really matters for your clients.. In this guide, we'll walk you through the steps. Therapynotes' psychiatry intake note template allows you to capture both a robust biopsychosocial history of your patient and effectively document medical services within a. Mentalyc notes cover symptoms, functioning, and include related quotes from the client, effectively conveying patient experiences as per guidewell's guidelines. To highlight documentation styles and content, this. To highlight documentation styles and content, this example contains a mix of narrative and bulleted information for each category within a template. Take advantage of our template library and focus your time where it really matters for your clients. Optimize your practice with an intake form template for therapists. This includes creating and providing useful counseling toolkits, resources, and templates. Unlike progress notes that track progress on ongoing treatment, intake notes are more comprehensive and capture the client's history, current situation, and treatment goals. Optimize your practice with an intake form template for therapists. In this guide, we'll walk you through the steps. A therapy intake assessment note is a structured document used by mental health professionals to collect and. Optimize your practice with an intake form template for therapists. Therapynotes’ intake note allows you to document a full biopsychosocial evaluation of your client, including the presenting problem, a mental status exam, and history. Templates for intake, progress notes, treatment plans and more! Each of these follow the same. Mentalyc's template builder is a powerful tool that allows therapists to. This includes creating and providing useful counseling toolkits, resources, and templates such as free counseling templates, free soap notes templates, and free counseling. Therapynotes’ intake note allows you to document a full biopsychosocial evaluation of your client, including the presenting problem, a mental status exam, and history. Each of these follow the same. A therapy intake assessment note is a. Mentalyc's template builder is a powerful tool that allows therapists to create customized progress and intake note templates. Intake questionnaires are forms that you send to clients, while treatment notes are forms you use internally to make notes on a client's timeline. Optimize your practice with an intake form template for therapists. This includes creating and providing useful counseling toolkits, resources, and templates such as free counseling templates, free soap notes templates, and free counseling. Take advantage of our template library and focus your time where it really matters for your clients. Therapynotes’ intake note allows you to document a full biopsychosocial evaluation of your client, including the presenting problem, a mental status exam, and history. To highlight documentation styles and content, this example contains a mix of narrative and bulleted information for each category within a template. Each of these follow the same. Mentalyc notes cover symptoms, functioning, and include related quotes from the client, effectively conveying patient experiences as per guidewell's guidelines. Unlike progress notes that track progress on ongoing treatment, intake notes are more comprehensive and capture the client's history, current situation, and treatment goals. Templates for intake, progress notes, treatment plans and more! A therapy intake assessment note is a structured document used by mental health professionals to collect and organize information about a new client during the initial intake.Nutrition Intake Form Template New 30 Blank Soap Note with Soap Report
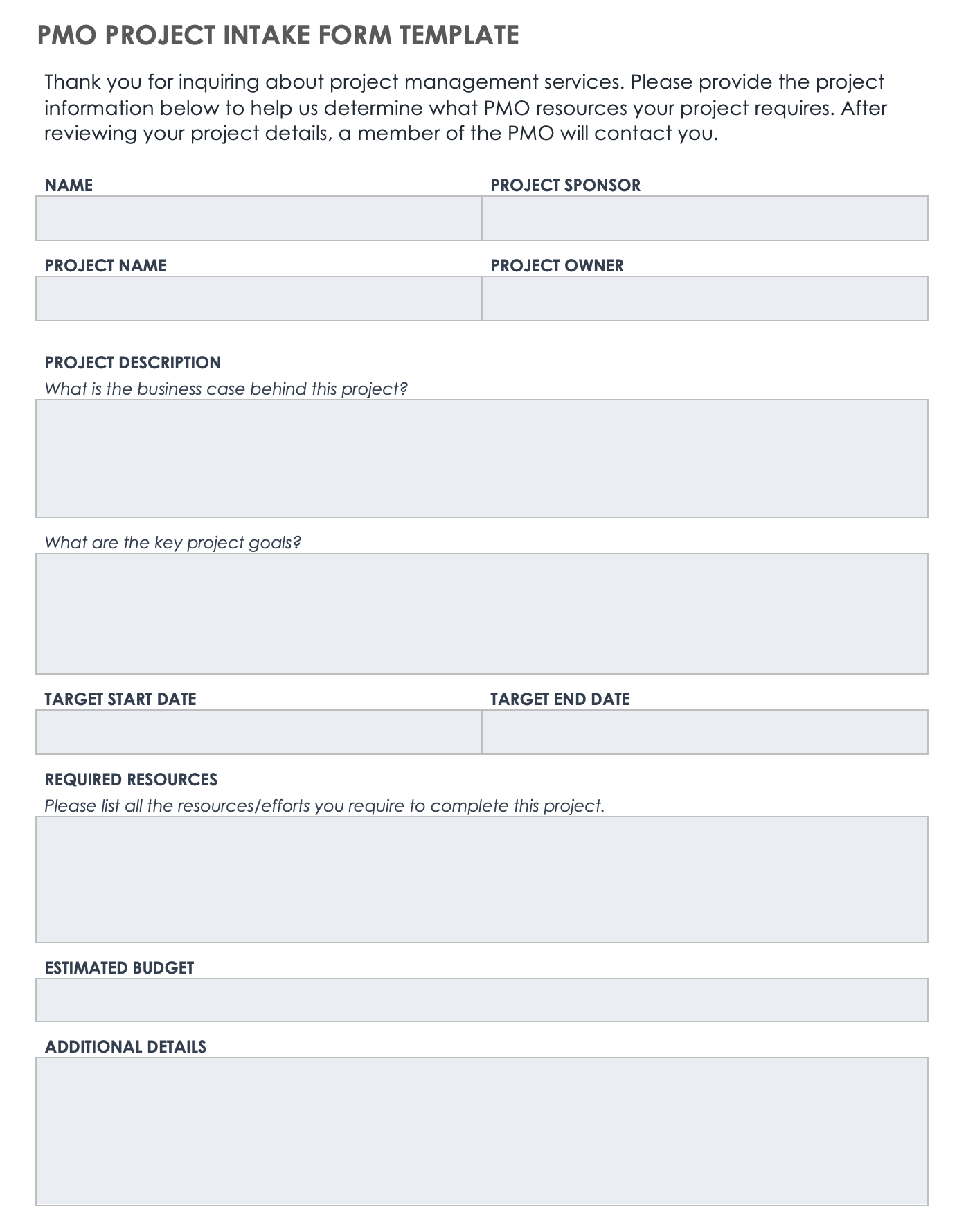
Intake Form Template Excel
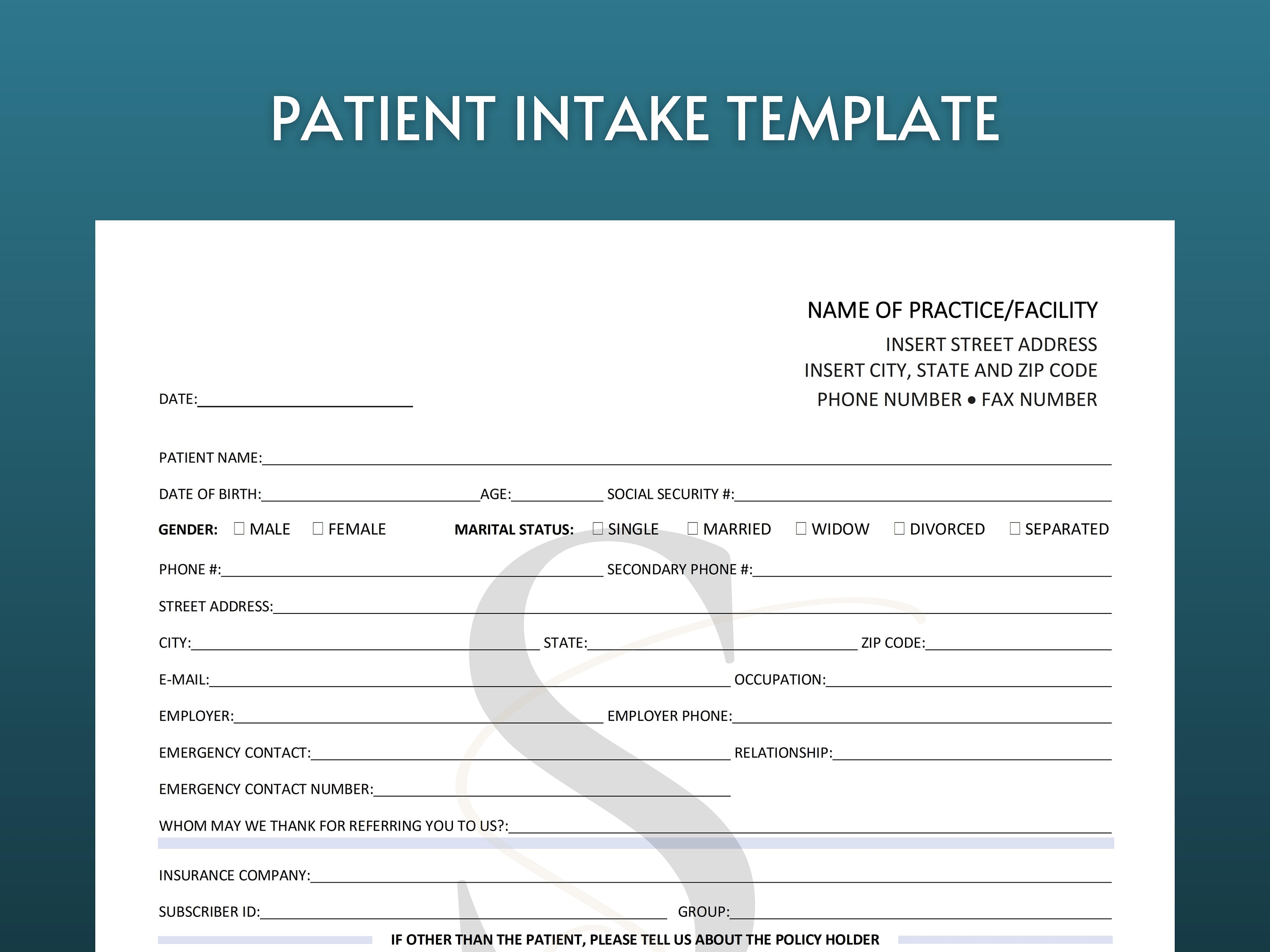
Medical Intake Form How to create a Medical Intake Form? Download
Case Management Intake form Template Beautiful Luxury Case Notes
Printable New Patient Intake Form Digital Download Patient Etsy UK
√ 24 Counseling Intake forms Templates in 2020 Templates, Counseling
Mental Health Intake Form & Template Free PDF Download
Complete an Intake Note TherapyNotes Help Center
√ 30 Medical Intake forms Template Effect Template Medical history
Simple New Client Intake Form (Canva Template) The Practice Lab
The Intake Assessment Template Simplifies The Initial Evaluation Process, Enabling Quick And Comprehensive Capture Of Essential Patient History And Primary Concerns.
Therapynotes' Psychiatry Intake Note Template Allows You To Capture Both A Robust Biopsychosocial History Of Your Patient And Effectively Document Medical Services Within A.
In This Guide, We'll Walk You Through The Steps.
Collect Vital Client Info And Ensure A Smooth Therapy Process.
Related Post:




.png)


