Psychiatry Hpi Template
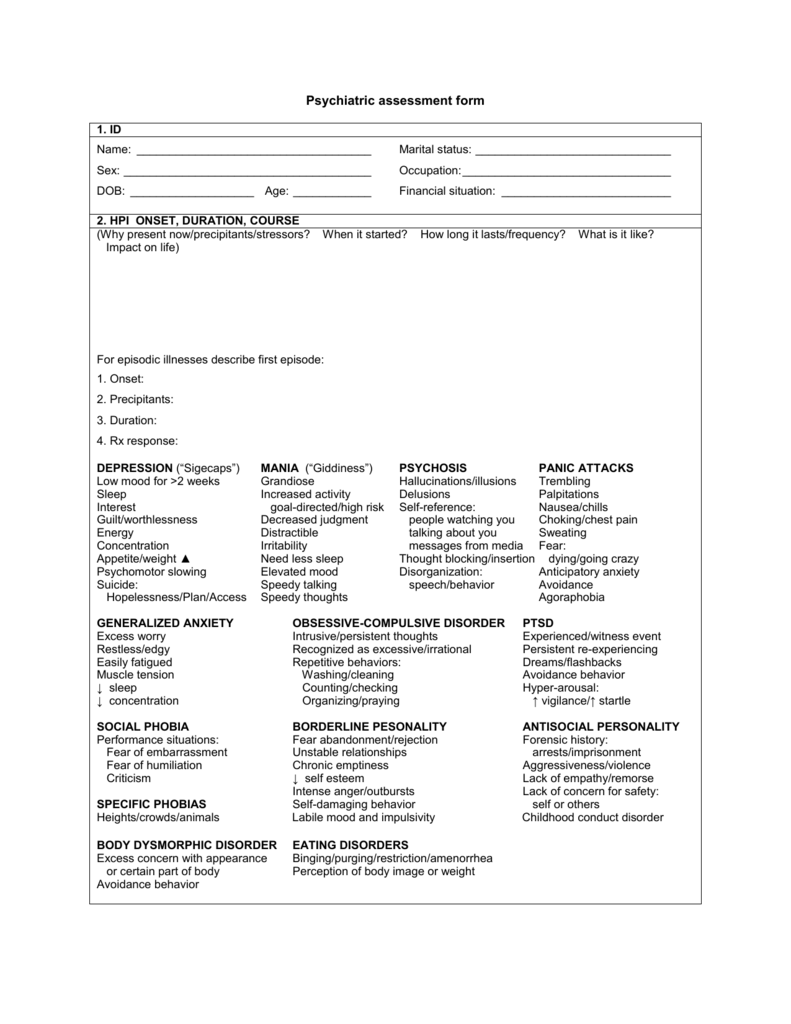
Psychiatry Hpi Template - A note template for taking a psychiatric history and physical. Psychiatry progress note templates to streamline your practice. What should you include in your initial psychiatric evaluation? Trying to see what the best intake guide or sheet you've had or utilized to interview a patient during your psychiatry rotation. Quality, severity, duration, timing, context, modifying factors, associated signs and symptoms): Each template can be customized to fit individual needs, and. Osmind simplifies the process of writing psychiatry progress notes with over 60 templates tailored to for mental health clinicians. As a mental health practitioner, you will come across a myriad of diverse documentation templates in the course of your professional endeavors: You’ll want to have a template that includes the following sections: Found this from matchpsychiatry and was going to. Learn how to use the new system template to document psychiatric/psychological assessment and initial inpatient care in the individual progress note and crisis progress note. Incorporate elements of the pmh, fh and sh relevant to the patient’s story. The template provides guidance on what to include in each section, such as ensuring a thorough medical review of systems, asking about family psychiatric history, and including discharge. (document at least 4 of the following elements of the present illness: What should you include in your initial psychiatric evaluation? The history of present illness (hpi) component of an e/m service is comprised of eight elements: Each template can be customized to fit individual needs, and. As a mental health practitioner, you will come across a myriad of diverse documentation templates in the course of your professional endeavors: Osmind simplifies the process of writing psychiatry progress notes with over 60 templates tailored to for mental health clinicians. Found this from matchpsychiatry and was going to. Incorporate elements of the pmh, fh and sh relevant to the patient’s story. Learn how to use the new system template to document psychiatric/psychological assessment and initial inpatient care in the individual progress note and crisis progress note. Psychiatry progress note templates to streamline your practice. What should you include in your initial psychiatric evaluation? The physician conducted a psychiatric. Discover a structured mental health evaluation note template tailored for psychiatrists. A note template for taking a psychiatric history and physical. Chief complaint (this can be in the patient’s own words or a. The physician conducted a psychiatric evaluation of a patient who. As a mental health practitioner, you will come across a myriad of diverse documentation templates in the. Found this from matchpsychiatry and was going to. Each template can be customized to fit individual needs, and. The physician conducted a psychiatric evaluation of a patient who. Chief complaint (this can be in the patient’s own words or a. Quality, severity, duration, timing, context, modifying factors, associated signs and symptoms): Ideally, this should be in the patient’s words. Found this from matchpsychiatry and was going to. For psychiatrists, nurse practitioners, nurses, physician assistants, residents, and students. A note template for taking a psychiatric history and physical. Chief complaint (this can be in the patient’s own words or a. Include the primary symptom causing the patient to seek care. Trying to see what the best intake guide or sheet you've had or utilized to interview a patient during your psychiatry rotation. Incorporate elements of the pmh, fh and sh relevant to the patient’s story. The history of present illness (hpi) component of an e/m service is comprised of eight. Each template can be customized to fit individual needs, and. (document at least 4 of the following elements of the present illness: The template provides guidance on what to include in each section, such as ensuring a thorough medical review of systems, asking about family psychiatric history, and including discharge. For psychiatrists, nurse practitioners, nurses, physician assistants, residents, and students.. Psychiatry progress note templates to streamline your practice. Includes comprehensive sections like hpi, mse, risk assessment, diagnosis, and treatment plan with. The physician conducted a psychiatric evaluation of a patient who. You’ll want to have a template that includes the following sections: Osmind simplifies the process of writing psychiatry progress notes with over 60 templates tailored to for mental health. Include the primary symptom causing the patient to seek care. (document at least 4 of the following elements of the present illness: Psychiatry progress note templates to streamline your practice. You’ll want to have a template that includes the following sections: What should you include in your initial psychiatric evaluation? Discover a structured mental health evaluation note template tailored for psychiatrists. Psychiatry progress note templates to streamline your practice. Incorporate elements of the pmh, fh and sh relevant to the patient’s story. The physician conducted a psychiatric evaluation of a patient who. A note template for taking a psychiatric history and physical. The physician conducted a psychiatric evaluation of a patient who. As a mental health practitioner, you will come across a myriad of diverse documentation templates in the course of your professional endeavors: Discover a structured mental health evaluation note template tailored for psychiatrists. The history of present illness (hpi) component of an e/m service is comprised of eight elements: Quality,. For psychiatrists, nurse practitioners, nurses, physician assistants, residents, and students. Found this from matchpsychiatry and was going to. The template provides guidance on what to include in each section, such as ensuring a thorough medical review of systems, asking about family psychiatric history, and including discharge. Osmind simplifies the process of writing psychiatry progress notes with over 60 templates tailored to for mental health clinicians. Include the primary symptom causing the patient to seek care. Includes comprehensive sections like hpi, mse, risk assessment, diagnosis, and treatment plan with. Trying to see what the best intake guide or sheet you've had or utilized to interview a patient during your psychiatry rotation. Each template can be customized to fit individual needs, and. Learn how to use the new system template to document psychiatric/psychological assessment and initial inpatient care in the individual progress note and crisis progress note. Discover a structured mental health evaluation note template tailored for psychiatrists. Ideally, this should be in the patient’s words. A note template for taking a psychiatric history and physical. Psychiatry progress note templates to streamline your practice. Quality, severity, duration, timing, context, modifying factors, associated signs and symptoms): You’ll want to have a template that includes the following sections: As a mental health practitioner, you will come across a myriad of diverse documentation templates in the course of your professional endeavors:Psychiatry Hpi Template Master of Documents
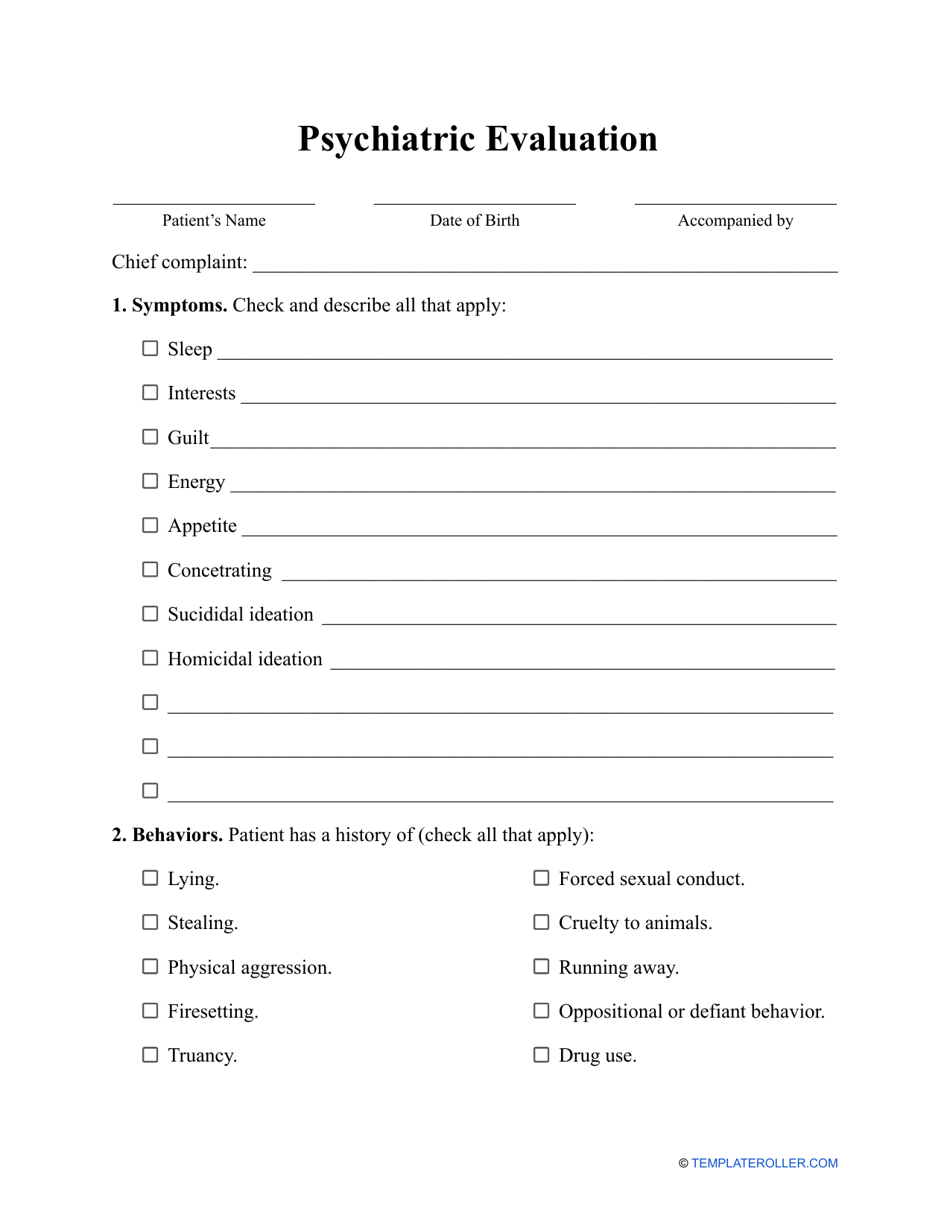
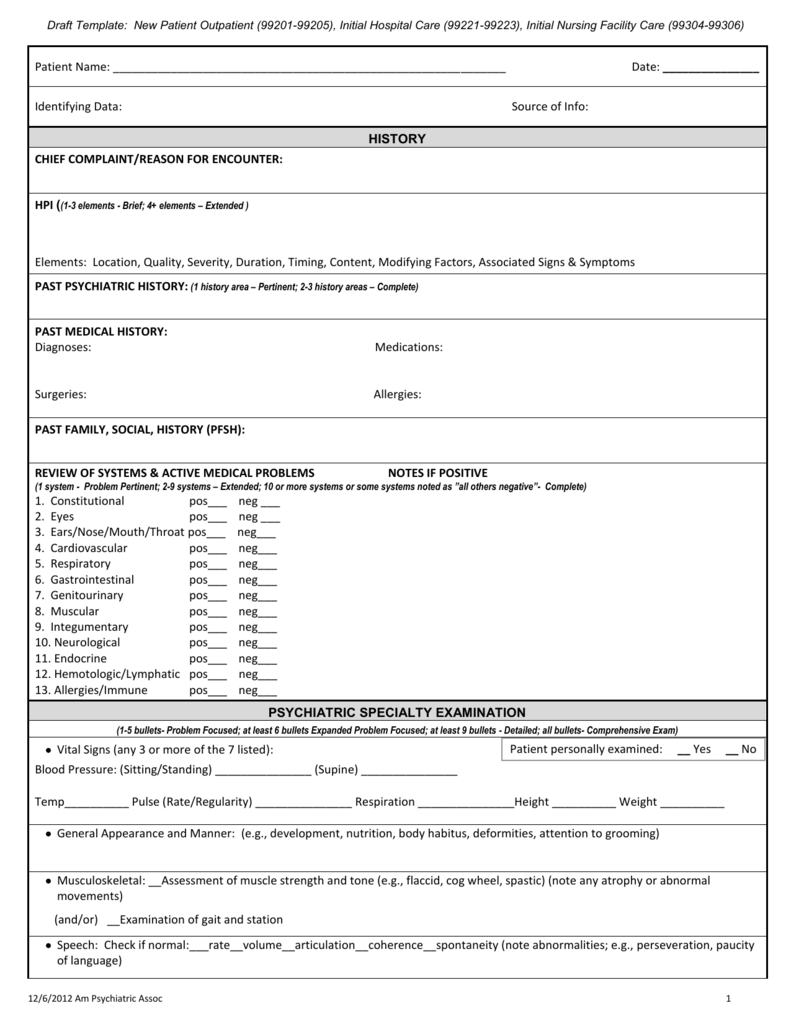
Psychiatric Evaluation Template Download Printable PDF Templateroller
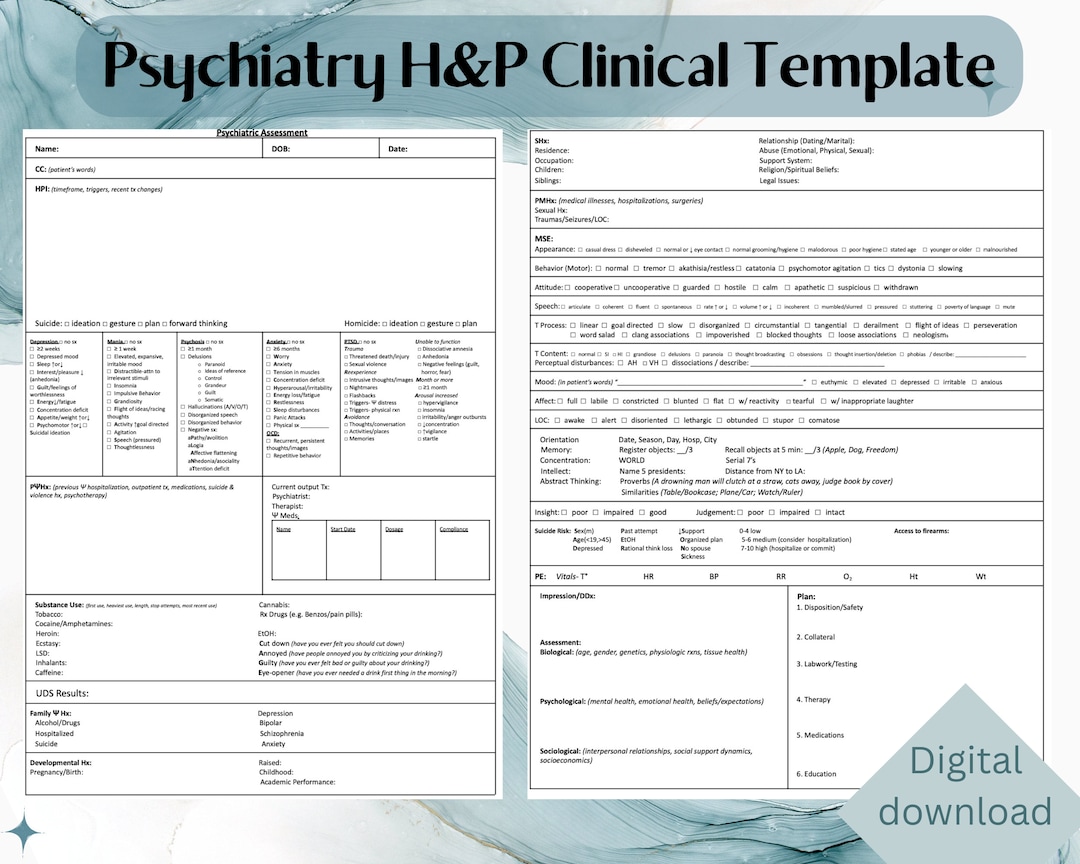
Psychiatric Assessment (Editable, Fillable, Printable PDF
Psychiatry H&P Clinical Template for Medical Students and Healthcare
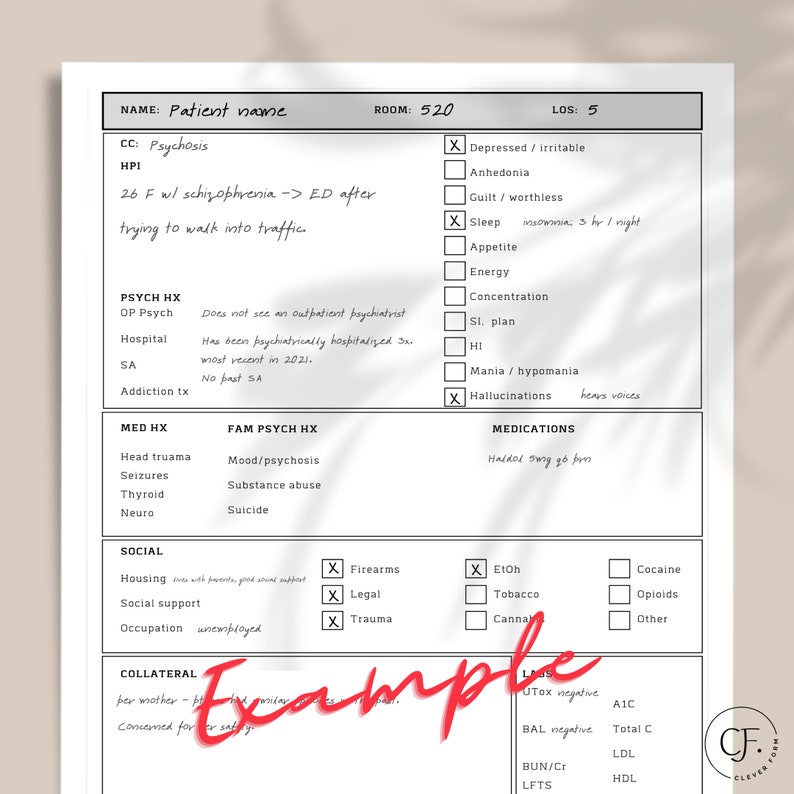
Psychiatry HPI Template Psych History and Physical Questions for
Psychiatry Hpi Template Master of Documents
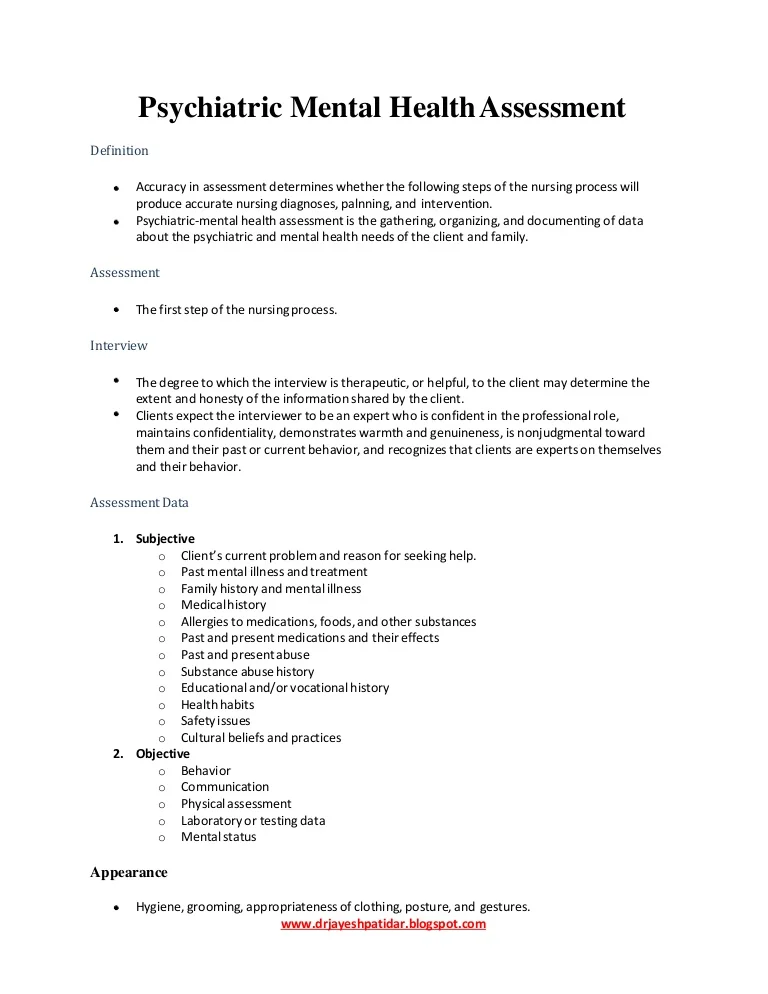
Psychiatric mental health assessment
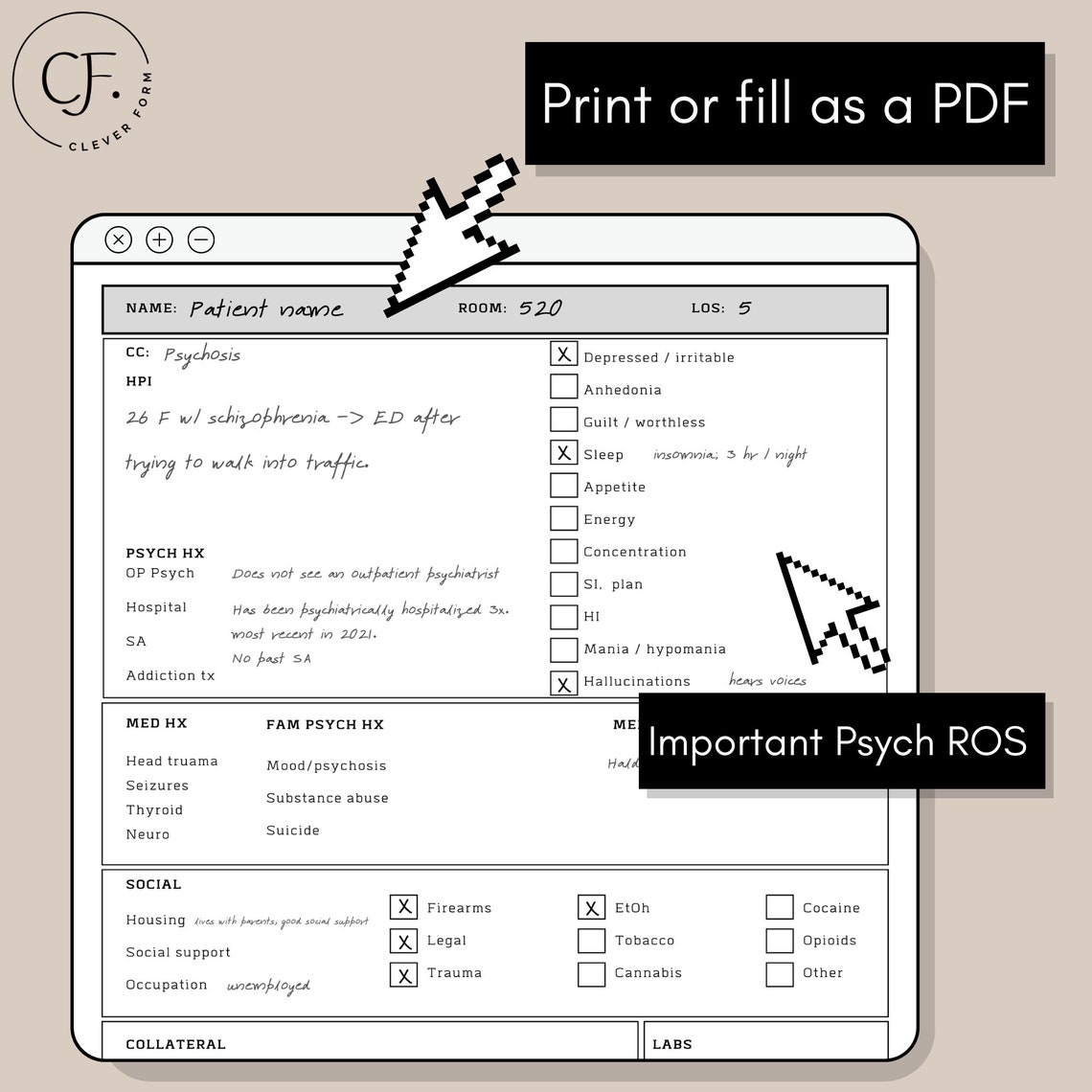
Psychiatric Initial Evaluation Template
Psychiatry HPI Template Psych History and Physical Questions for
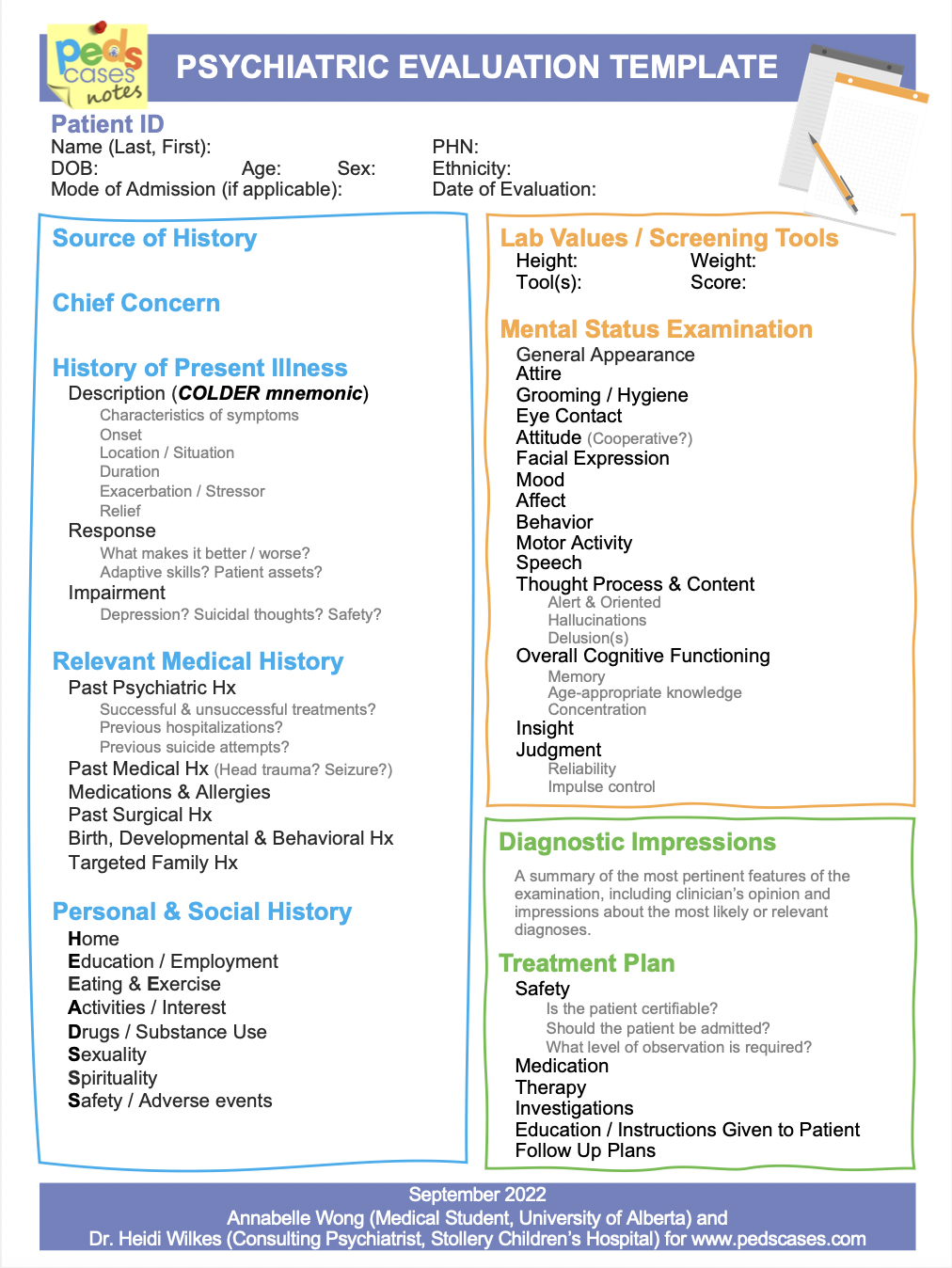
Psychiatric Evaluation Template PedsCases
The Physician Conducted A Psychiatric Evaluation Of A Patient Who.
Incorporate Elements Of The Pmh, Fh And Sh Relevant To The Patient’s Story.
(Document At Least 4 Of The Following Elements Of The Present Illness:
The History Of Present Illness (Hpi) Component Of An E/M Service Is Comprised Of Eight Elements:
Related Post: