Psychotherapy Progress Notes Template
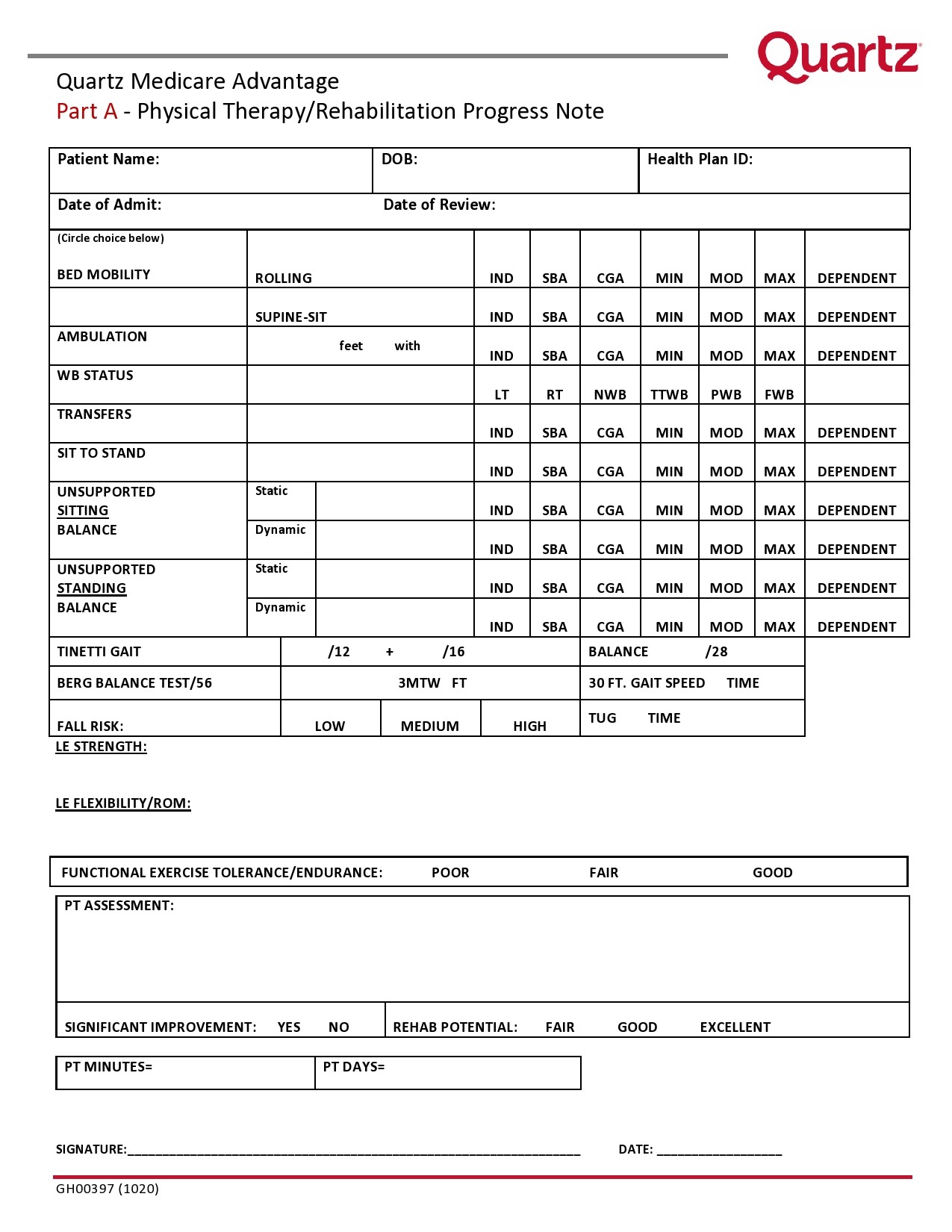
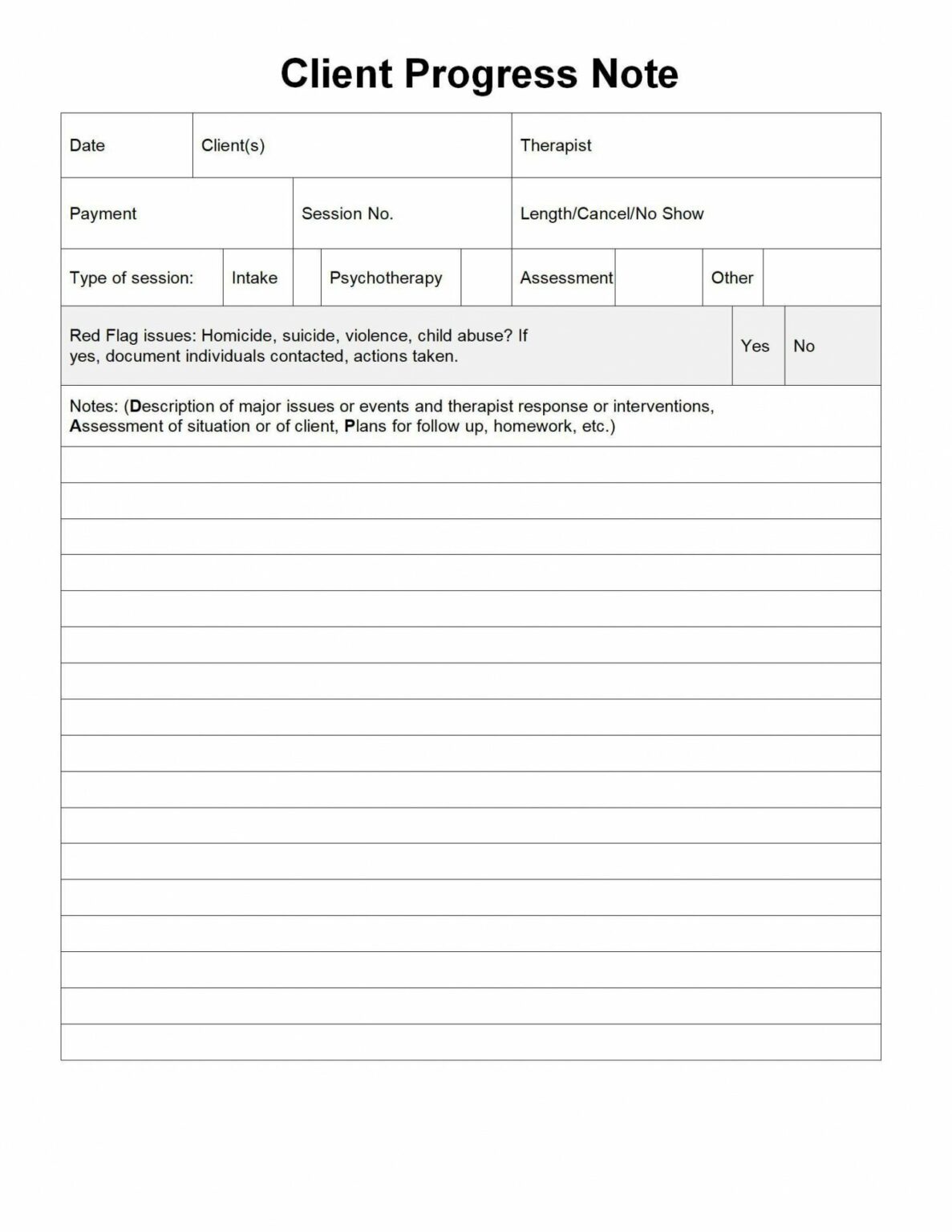
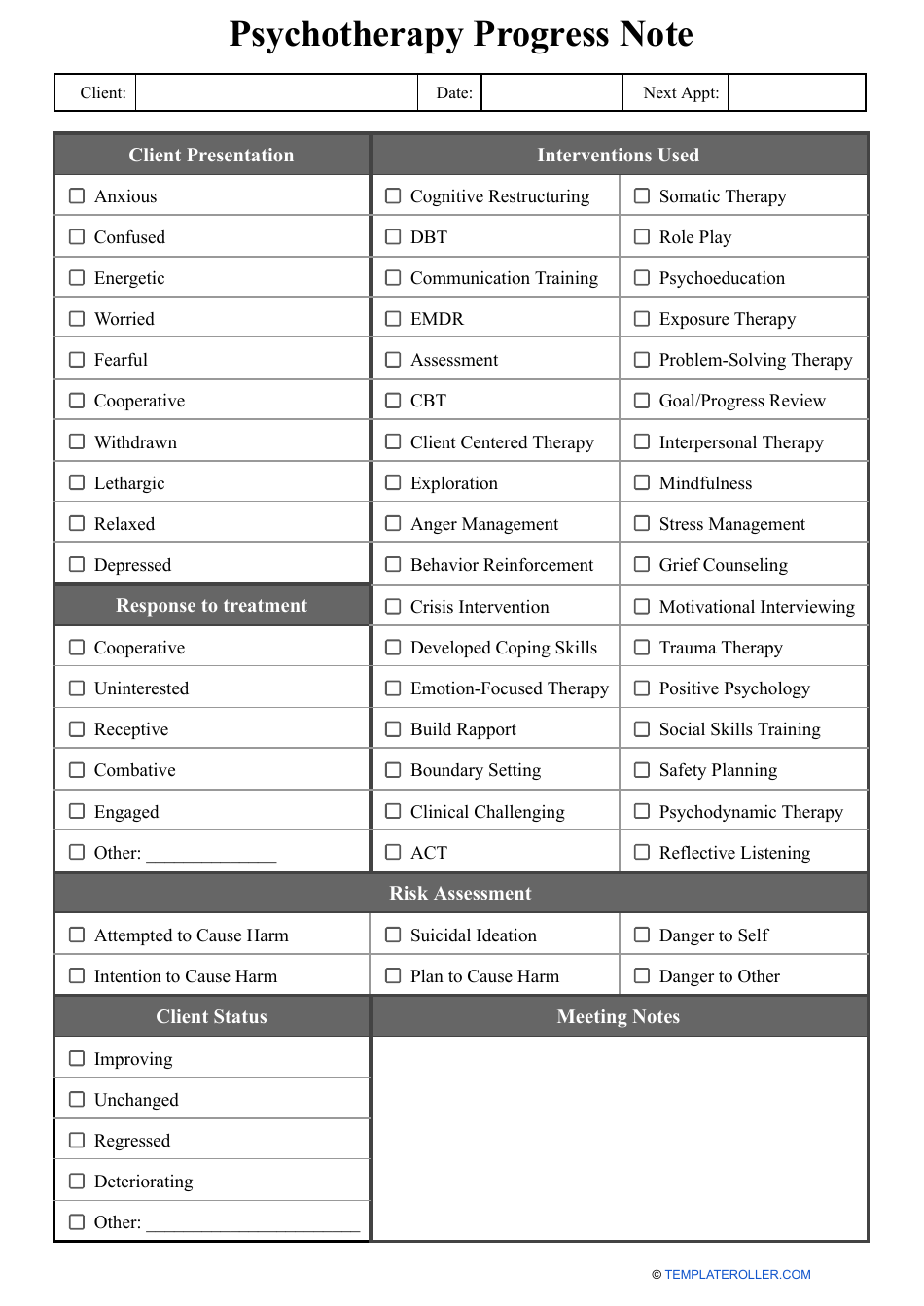
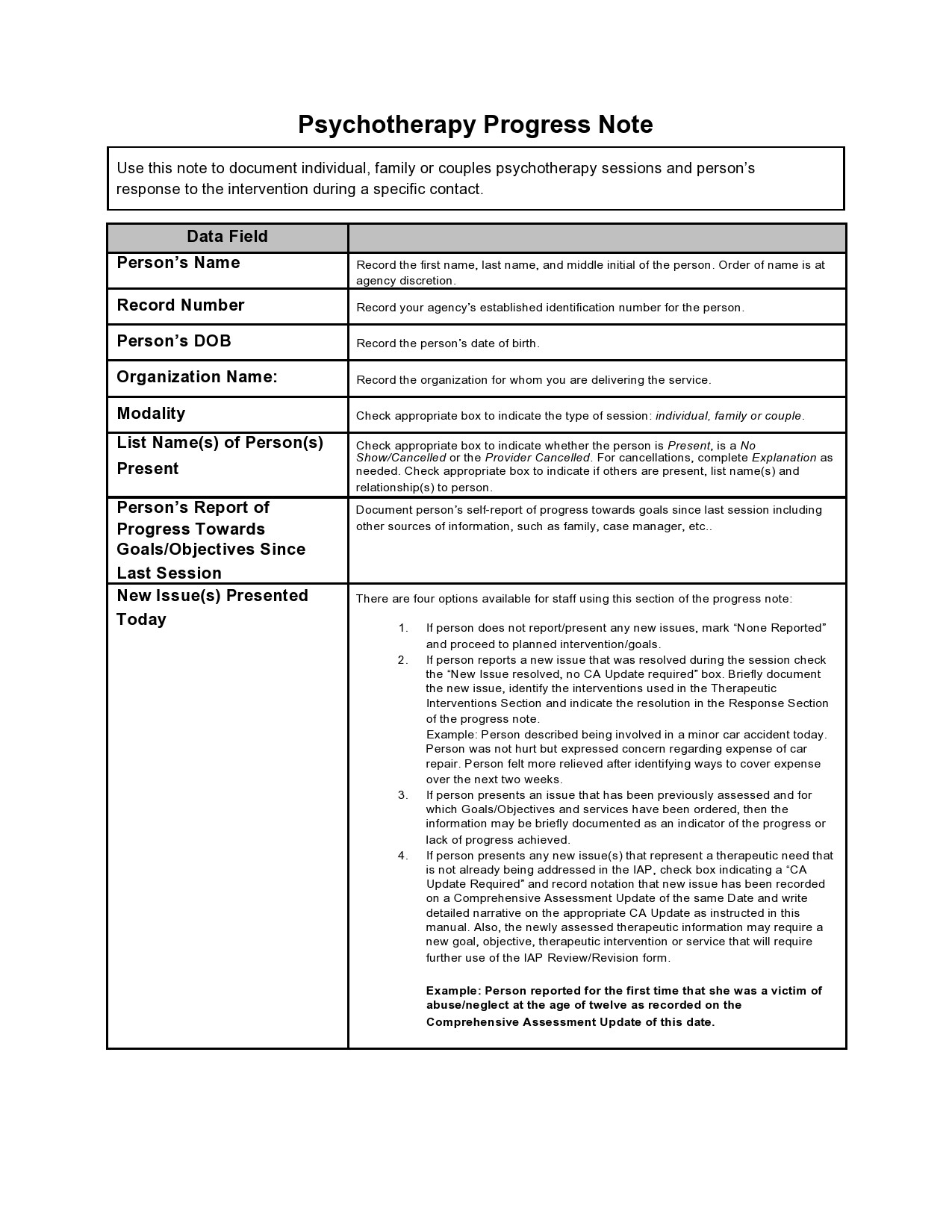
Psychotherapy Progress Notes Template - As a provider you can always contact the health plan, request an outline of the questions that will be asked, and ask for the plan’s medical necessity criteria. Under hipaa, process notes (or “psychotherapy notes”) are more strictly regulated than any other client records. Documenting therapy sessions in the golden thread: Soap notes are one form of medical record documentation, and the soap format is incorporated in the templates provided. Progress notes are also required for video telehealth sessions. If you have a client contact between sessions that is not a billable service or a therapy session, you can document that using the phone/email consultation template. Phone/email consultation note template ; as a resource for sondermind providers, we’ve created an intake template that you can access here. Discharge summary template help change the future of mental health care. To help you fill out an intake template, we’ve also developed sample intake documents featuring fictional clients. Avoid expanding beyond what is required for each section. Think of them as cliff notes of the very personal and confidential conversations you have with your client, only meant to. Treatment review tips request information about a review: Progress note template help change the future of mental health care. Wrap up the session by summarizing the interview, providing initial case formulation, positively reinforcing their decision to seek professional services, and explaining how the second visit will look. These notes provide evidence of medical necessity and should be used throughout the intake and treatment process. Below are the required components to. Join thousands of mental health clinicians changing the way people access, receive, and participate in their treatment. If you have a client contact between sessions that is not a billable service or a therapy session, you can document that using the phone/email consultation template. Progress notes use the soap format, and a risk assessment and mental status notation further strengthen the documentation. To help you fill out an intake template, we’ve also developed sample intake documents featuring fictional clients. Phone/email consultation note template ; Documenting end of care in the golden thread: as a resource for sondermind providers, we’ve created an intake template that you can access here. Remember, there is no such thing as the perfect progress note! Treatment review tips request information about a review: as a resource for sondermind providers, we’ve created an intake template that you can access here. If you have a client contact between sessions that is not a billable service or a therapy session, you can document that using the phone/email consultation template. Documenting therapy sessions in the golden thread: Join thousands. As a provider you can always contact the health plan, request an outline of the questions that will be asked, and ask for the plan’s medical necessity criteria. Join thousands of mental health clinicians changing the way people access, receive, and participate in their treatment. Documentation requirements specific to video telehealth. Documenting therapy sessions in the golden thread: Remember, there. Phone/email consultation note template ; Treatment review tips request information about a review: If you have a client contact between sessions that is not a billable service or a therapy session, you can document that using the phone/email consultation template. Remember, there is no such thing as the perfect progress note! In the event one of your clients and their. Soap notes are one form of medical record documentation, and the soap format is incorporated in the templates provided. Under hipaa, process notes (or “psychotherapy notes”) are more strictly regulated than any other client records. Progress notes are also required for video telehealth sessions. The samples contain a mix of narrative and bulleted information for each category in the template.. As a provider you can always contact the health plan, request an outline of the questions that will be asked, and ask for the plan’s medical necessity criteria. Psychotherapy notes are those notes you take during a session with your client, for your own safekeeping. as a resource for sondermind providers, we’ve created an intake template that you can access. Join thousands of mental health clinicians changing the way people access, receive, and participate in their treatment. Remember, there is no such thing as the perfect progress note! as a resource for sondermind providers, we’ve created an intake template that you can access here. Discharge summary template help change the future of mental health care. Below are the required components. Under hipaa, process notes (or “psychotherapy notes”) are more strictly regulated than any other client records. Psychotherapy notes are those notes you take during a session with your client, for your own safekeeping. The samples contain a mix of narrative and bulleted information for each category in the template. If you have a client contact between sessions that is not. Discharge summary template help change the future of mental health care. Documentation requirements specific to video telehealth. If you have a client contact between sessions that is not a billable service or a therapy session, you can document that using the phone/email consultation template. Progress note template help change the future of mental health care. Under hipaa, process notes (or. Under hipaa, process notes (or “psychotherapy notes”) are more strictly regulated than any other client records. Join thousands of mental health clinicians changing the way people access, receive, and participate in their treatment. In the event one of your clients and their progress notes are ever reviewed by insurance keep these suggestions in mind: Phone/email consultation note template ; Wrap. Progress notes are also required for video telehealth sessions. To help you fill out an intake template, we’ve also developed sample intake documents featuring fictional clients. Documenting end of care in the golden thread: as a resource for sondermind providers, we’ve created an intake template that you can access here. Think of them as cliff notes of the very personal and confidential conversations you have with your client, only meant to. Join thousands of mental health clinicians changing the way people access, receive, and participate in their treatment. Discharge summary template help change the future of mental health care. Remember, there is no such thing as the perfect progress note! Under hipaa, process notes (or “psychotherapy notes”) are more strictly regulated than any other client records. Avoid expanding beyond what is required for each section. If you have a client contact between sessions that is not a billable service or a therapy session, you can document that using the phone/email consultation template. Psychotherapy notes are those notes you take during a session with your client, for your own safekeeping. These notes provide evidence of medical necessity and should be used throughout the intake and treatment process. Documenting therapy sessions in the golden thread: The samples contain a mix of narrative and bulleted information for each category in the template. Treatment review tips request information about a review:40 Free Therapy Notes Templates (Progress Notes) ᐅ TemplateLab
Editable Psychotherapy Progress Note Template Addictionary Group
Psychotherapy Progress Note Template Download Printable PDF
40 Free Therapy Notes Templates (Progress Notes) ᐅ TemplateLab
40 Free Therapy Notes Templates (Progress Notes) ᐅ TemplateLab
Free Therapy Progress Note Template
40 Free Therapy Notes Templates (Progress Notes) ᐅ TemplateLab
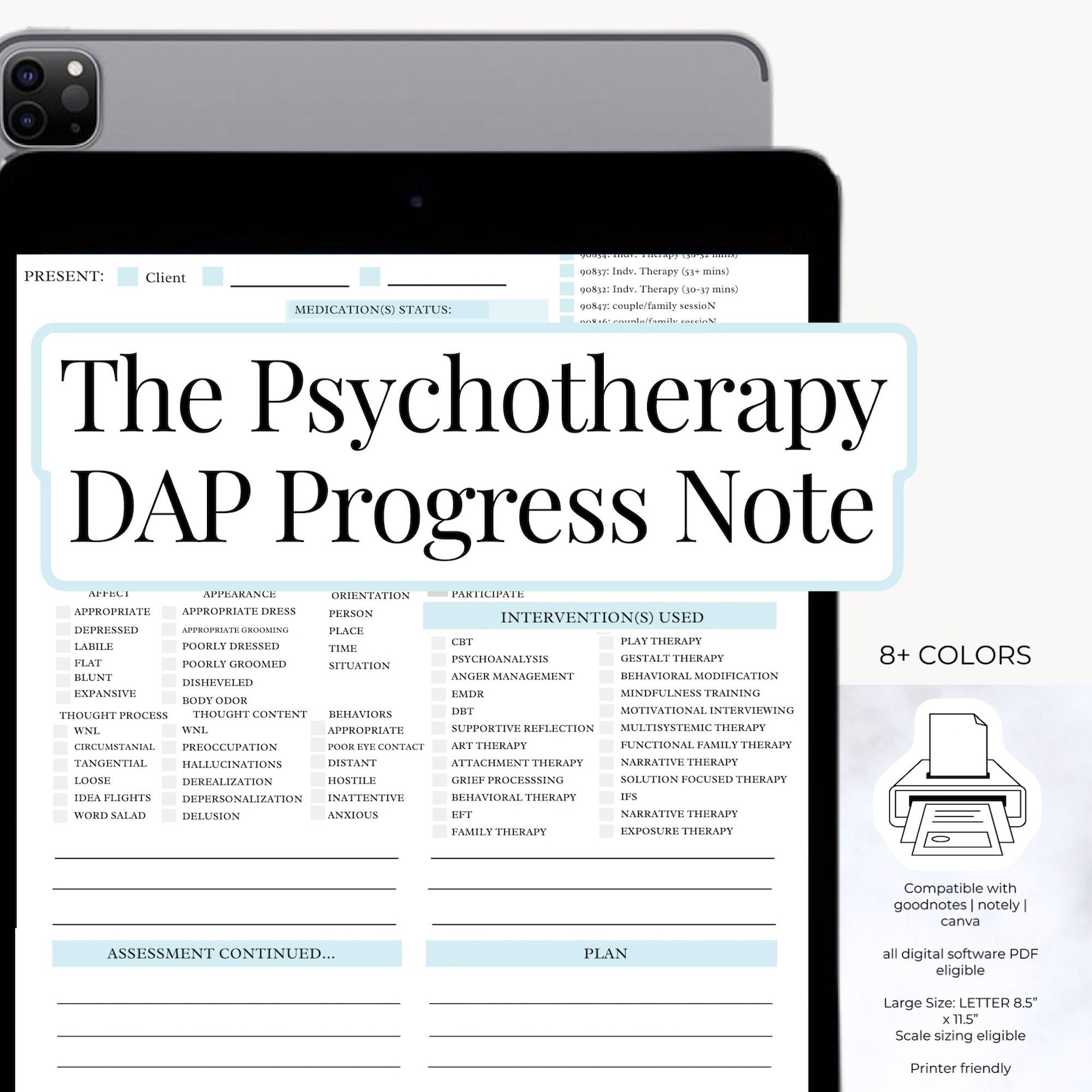
DAP Note Psychotherapy PROGRESS Note Template With MSE Etsy
Therapy Progress Notes and Goals (Editable, Fillable, Printable PDF
40 Free Therapy Notes Templates Progress Notes TemplateLab Fillable
Below Are The Required Components To.
Soap Notes Are One Form Of Medical Record Documentation, And The Soap Format Is Incorporated In The Templates Provided.
Progress Notes Use The Soap Format, And A Risk Assessment And Mental Status Notation Further Strengthen The Documentation.
Documentation Requirements Specific To Video Telehealth.
Related Post: